Short Scar Abdominoplasty & Mini Tummy Tuck in Sydney
Sydney Plastic Surgeon Mini Tummy Tuck Short Scar Abdominoplasty
Dr Gavin Sandercoe is an experienced Specialist Plastic Surgeon in Sydney and receives many questions about shorter scar abdominoplasty and mini tummy tucks. Both operations have their role and their ideal patients, but many patients elect to have a traditional or full abdominoplasty once they understand the difference and what they are missing out on.
Definitions
- Abdominoplasty is a several step operation to re-shape the abdominal wall.
- Incision (scar) in the lower abdominal wall, position & length varies between surgeons and patient factors
- Lifting the abdominal skin and fat off the abdominal muscles. The usual pattern is to undermine all the way from the pubic bone to the lower margin of the rib cage.
- Repair of separation of the abdominal muscles, and any midline hernias
- Shaping of the remaining abdominal fat through liposuction or direct removal
- Reposition the umbilicus, and closure of the lower abdominal scar
- Mini – abdominoplasty
- The abdominal skin & fat is only raised to the umbilicus
- Any rectus divarication is usually not repaired
- Short scar abdominoplasty
- Same as the standard abdominoplasty, but the incision (scar) is kept to between the anterior superior iliac spines (ASIS) – the bony point at the front of your pelvic brim. Once your incision/scar is even 1cm longer than these anatomical points, your procedure is now termed (by default) a long scar or standard abdominoplasty. Keeping within these two points often necessitates a slightly higher scar or results in a floating vertical scar where your umbilicus (belly button) used to be.
What abdominal changes occur with pregnancy?
As a woman goes through her pregnancy, her uterus enlarges and pushes out of the pelvis and into the abdominal cavity. This creates pressure and stretch within the contained space of the abdominal cavity. Similar processes occur when patients continue to develop intra-abdominal fat that stretches the abdominal wall (obesity) or have intra-abdominal masses or tumours.
There is some capacity for muscles to stretch to accommodate this abdominal volume. At a certain point, the muscles have stretched as far as they can, and the tendons and ligaments need to stretch to allow continuing expansion. The point at when this occurs depends on the total volume of abdominal mass, speed of stretch being applied, as well as genetic factors. There are two inter-linked ways for the body to allow continuing stretch – separation of the rectus muscles (rectus divarication) and increasing the distance between the bony restraints (pelvic brim and rib cage) by opening that angle by increasing the curve in the lower back. There is some stretch at the pubic symphysis (midpoint of the pelvis at the front), but this is more important in child birth than foetal growth. Rectus divarication is more common after pregnancy, so it is highly likely that hormonal factors are part of how and why this happens.
The things that can’t change are the bony limits – pelvis, rib cage, spinal column. The muscle layer connecting these structures is where all the stretch happens. The umbilicus is about the midpoint of the xiphisternum (lower end of sternum) and the pubic symphysis – so it is at the point of maximum stretch.
What are the benefits of a short scar abdominoplasty?
The short scar (between ASIS points) gives a skilled surgeon enough access to repair a rectus divarication along its full length, and shape the remaining fat in the abdominal wall. Increasing the scar length is performed to allow excision of extra skin and fat, and allow the scar to settle more evenly. The more work that is requested on the flanks, and the greater the amount of stretch marks, the more likely it is that a patient will get a better result from a longer scar.
Dr Gavin Sandercoe discusses the individual risks and benefits of short vs. long scar options with each abdominoplasty patient that he assesses, and allows them to choose the option that suits them best.
Why is mini-abdominoplasty a bad choice of operation for mothers?
The concept of a mini-abdominoplasty after pregnancy is like seeing a crack in your wall, but painting over it only without repairing the plaster crack.
Consider stretching a pair of swimmers. Despite pulling at a certain point most of the time, the elastic all the way around stretches. An equivalent change occurs with abdominal stretch. It is highly uncommon for women to only separate their abdominal muscles below the umbilicus, even if they only have a small amount of excess skin. In fact, Dr Sandercoe has never seen this occur.
Repairing only the lower abdominal rectus diastasis puts this area back to the tension that it should be in, but allows the upper abdominal area to stay lax and become an area of relative weakness. Women that have had mini-abdominoplasties report that with postural changes, eating or drinking, they get a bulge in their upper abdomen. They also do not gain the functional benefits of full rectus diastasis repair (decreased lower back pain, decreased stress incontinence).
Dr Sandercoe repairs several mini-abdominoplasties each year by converting them to full abdominoplasties and repairs the rectus diastasis all the way up to the xiphisternum. They rarely end up with a result that is as good as they could have had from accepting a standard (full) abdominoplasty as their original procedure.
Who is a good candidate for a mini-abdominoplasty?
The only good candidates for mini-abdominoplasty are young women whom have lost a moderate amount of weight and wish to look better, but do not wish to have a rectus divarication repair so as to allow pregnancies afterwards. Almost every other abdominoplasty patient has a better results from a standard or full abdominoplasty.
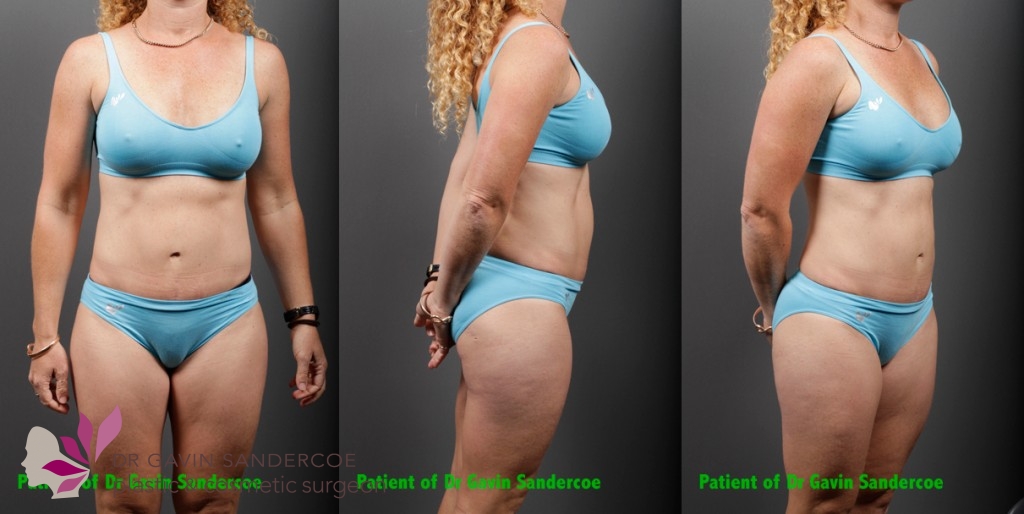
Case Studies
The following two patients were both mothers who might have been considered candidates for mini-abdominoplasty. After a discussion about the differences between a traditional and mini abdominoplasty, both patients elected to proceed with a standard abdominoplasty. Without a traditional abdominoplasty, the upper rectus divarication would not have been able to be repaired, and their final results would have been lessened and their functional improvements would have been reduced.
Patient A – 38 years old, BMI 21.3, 3cm rectus divarication, 305g abdominal wall removed

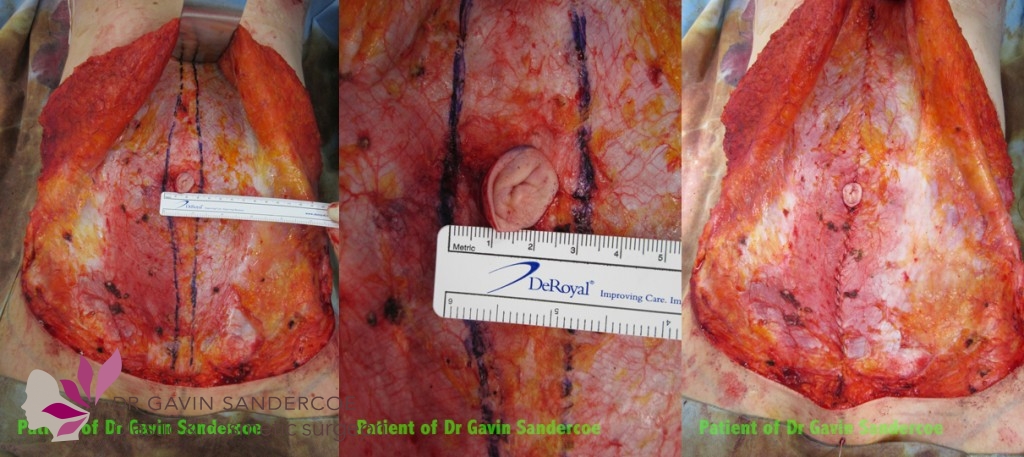

Patient B – 42 years old, BMI 23.5, 4cm rectus divarication, 200g abdominal wall removed


Patient Education Library