Umbilical Necrosis in Abdominoplasty
Umbilical Necrosis in Abdominoplasty
What is umbilical necrosis?
Necrosis is the medical term for tissue death. Umbilical necrosis is when the umbilical tissue dies, which usually occurs as part of a medical procedure such as an abdominoplasty.
How do Specialist Plastic Surgeons move an umbilicus during an abdominoplasty?
All steps within Plastic Surgery procedures require an understanding of blood supply, so that tissues heal rather than die. As the umbilicus is a scar, Specialist Plastic Surgeons understand that the blood supply to the umbilicus comes from both the surrounding abdominal skin as well as from the abdominal muscle layer. These two blood supplies are termed superficial (skin) and deep (muscle).
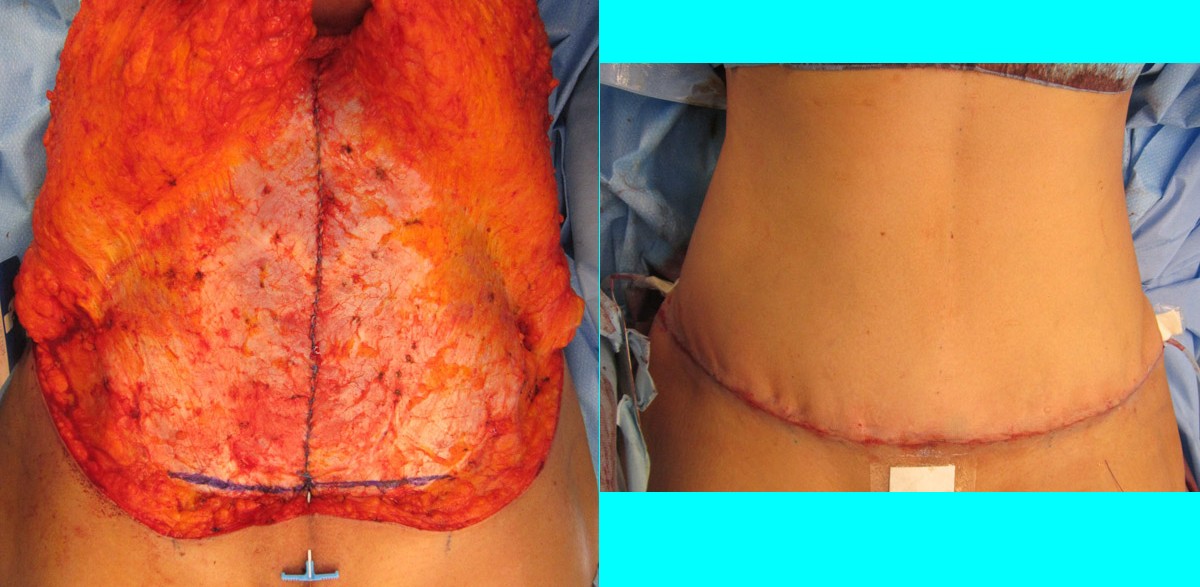
During most abdominoplasties, Specialist Plastic Surgeons will dissect out the umbilicus down to the abdominal wall. This disconnects the blood supply from the abdominal skin (superficial) and isolates the umbilicus on the blood supply from the muscle layer (deep). In rare circumstances, the opposite technique is used. Leaving the umbilicus attached to the abdominal skin and disconnecting it from the linea alba is termed an “umbilical float”. Umbilical floats are only useful in patients with minimal skin laxity AND an umbilicus that naturally sits abnormally high.
What happens if the deep blood supply to the umbilicus is inadequate?
The deep blood supply to an umbilicus can be reduced several situations. The most common is the prior use of the umbilicus as an access port for laparascopy (or multiple laparoscopies), or other general surgical procedures. Some surgeons will incise in and around the umbilicus, and the umbilical stalk can be completely divided during a laparoscopy approach.
A second reason that the deep blood supply to an umbilicus can be reduced is if the Specialist Plastic Surgeon finds an umbilical or paraumbilical hernia that requires repair during your abdominoplasty. These hernias can be in combination with the scarring from past laparoscopies, which is a double whammy for the umbilical blood supply. Umbilical and paraumbilical hernias are also very common in ladies who have rectus diastasis from pregnancy.
Some Specialist Plastic Surgeons will not repair an umbilical or paraumbilical hernia at the same time as performing an abdominoplasty due to the increased risk of umbilical necrosis. It is Dr Gavin Sandercoe’s view that all midline hernias should be repaired during an abdominoplasty, as the access (view) of the hernias is much greater than that during a normal hernia repair. This allows a stronger and safer repair of those hernias. In the long run, a well repaired hernia and a planned umbilical reconstruction has less scarring on the abdomen than a normal umbilicus requiring a hernia repair after the abdominoplasty.

What happens if this altered blood supply is not predicted?
Alteration to the umbilical blood supply can be predicted preoperatively sometimes, but sometimes Specialist Plastic Surgeons only find out during your abdominoplasty. Your Specialist Plastic Surgeon is then in an awkward position – try to save the umbilicus or discard it & commit to an umbilical reconstruction.
It sounds tempting to attempt to save the umbilicus, but if it does not survive the chances of a good reconstruction fall greatly. Umbilical reconstructions look most normal if they are performed in fresh skin without tethering from prior scarring. Umbilical reconstructions should be staged about 3 months after an abdominoplasty so that the blood supply to the abdominal skin has recovered & normalised.
What can be done to salvage an umbilicus?
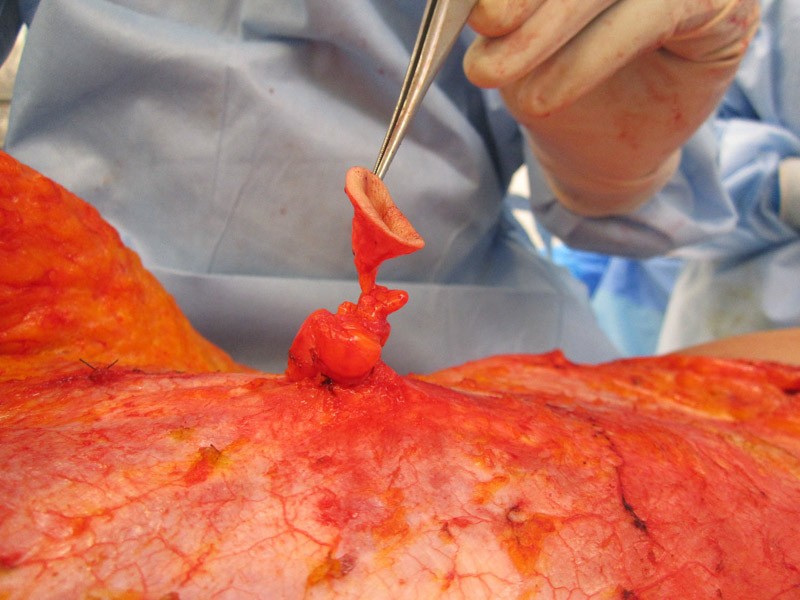
Once a Specialist Plastic Surgeon has raised the abdominal fat & skin off the muscle, they will have a reasonable assessment of the amount of risk to the umbilical blood supply during your abdominoplasty. If the umbilical stalk looks thin, scarred or otherwise dicey they will know that tough decisions might lay ahead. Repairing a rectus divarication will further reduce the blood supply but leaving space around the umbilical stalk helps reduce that impact. If an umbilical or paraumbilical hernia require repairing at the time, then a strong repair will reduce the amount of blood flowing into the umbilicus.
If the umbilicus looks to be in trouble during the operation, your surgeon can loosen the repair of any nearby hernias and rectus divarication. At that point, they need to make an assessment as to if the umbilicus looks like it will recover. It is Dr Gavin Sandercoe’s opinion that if the umbilicus does not pink up quickly, the best decision is to remove the umbilicus and plan for a reconstruction in 3 months. There are some Specialist Plastic Surgeons who prefer to reconstruct the umbilicus rather than using the native one (even when the blood supply is healthy & normal), so this is not a disaster!
Should the umbilicus look like it is going to recover, your Specialist Plastic Surgeon will inset the umbilicus like they would normally and finish your abdominoplasty. From this point onwards, it is a waiting game. If the umbilicus dies, then your surgeon will dress the wound until it heals. This may require a small procedure to remove any non-viable tissue to speed the healing. Your umbilicus may go through a phase where the outer layer of skin dies off and it heals from the deeper layers of skin.
If you are in Sydney and considering an abdominoplasty, we invite you to use the form below to contact the team at Dr Gavin Sandercoe Specialist Plastic Surgeon. All surgical procedures have some risk, and you should consider a second opinion from another Specialist Plastic Surgeon in Sydney.
Patient Education Library
This website contains information about cosmetic and plastic surgery procedures and is intended for persons 18 years of age or older.


